Abstract
Introduction
Cancer and its treatments are well-recognized risk factors for the development of venous thromboembolism (VTE). The occurrence of VTE has been associated with an increased mortality in patients with cancer. Here we retrospectively reviewed the incidence and characteristics of cancer-associated thrombosis (CAT) in a large cohort of cancer patients treated at our institution as well as compared treatment outcomes of this group of patients with a 1:1 matched pair group of cancer patients without CAT.
Methods
Data of consecutive patients, 18 years of age or older, with a newly diagnosis of both hematologic malignancies or solid tumors who diagnosed and treated either as an inpatient or outpatient setting at our institution between 2011 to 2015 were included in this analysis. Patients who received anticoagulants for the purpose of either prophylaxis or treatment within 2 weeks before cancer diagnosis and who did not have a histologically confirmed a cancer diagnosis or complete follow up data were excluded from the study.
To compare the outcomes of cancer patients with and without CAT, cancer patients who did not experience CAT were randomly selected from the same database and were matched individually (1:1) to cancer patients with CAT based on age, sex, cancer type and stage (limited or advanced) to form a matched cohort of patients as control.
Primary outcome was cumulative incidence of CAT at 6 months and 1 year after cancer diagnosis, while incidence of recurrent VTE, major and minor bleeding, relapse, non-relapse mortality (NRM), overall survival (OS) and progression-free survival (PFS) were analyzed as secondary outcomes.
CAT was defined as at least 1 site of venous thrombosis confirmed by imaging results, which occurred anytime after the initial diagnosis, during the treatment or follow-up.
Results
Total 2,291 newly diagnosed cancer patients (633 patients with hematologic malignancies and 1,658 patients with solid cancers) with a median age of 58 years (range 18-93 years) were included in the analysis.
CAT was developed in 83 patients (52 females and 31 males) with a median age of 61 year (range 20-85 years). The cumulative incidence of CAT at 6 months and 1 year was 2.7% and 3.4%, respectively. The median time from cancer diagnosis to the diagnosis of CAT was 3.2 months (range 1- 62 months).
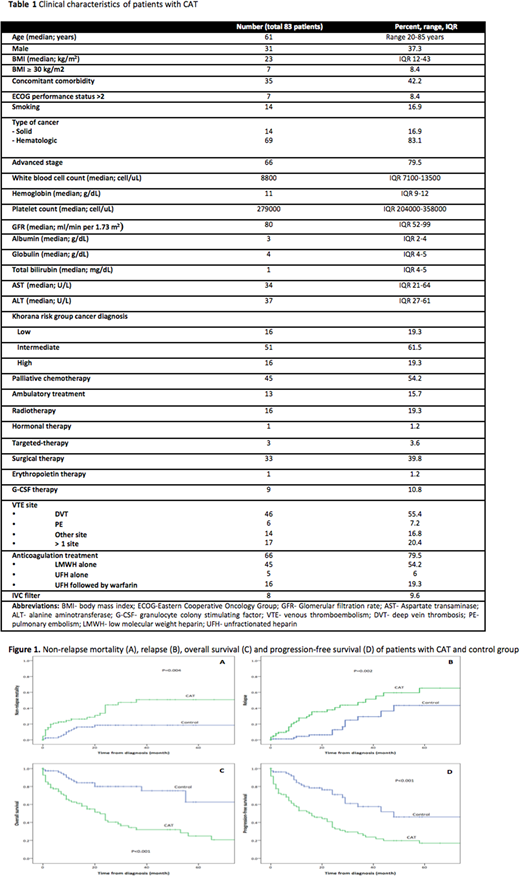
Sites of VTE were deep vein thrombosis in extremities (N=46; 55.4%), pulmonary embolism (N=6; 7.2%), splanchnic vein thrombosis (N=9; 10.8%) and cerebral venous sinus thrombosis (N=5, 6%). Seventeen patients (20%) developed more than 1 site of VTE. Sixty-nine (83%) cases with CAT were diagnosed in patients with hematologic malignancies including 35, 22 and 12 cases with lymphoma, acute leukemia and myeloproliferative neoplasms, respectively. Overall the incidence was 10.9% in hematologic malignancies and 0.8% in solid tumors. The majority of the CAT cases occurred in advanced stage cancers (66 patients; 79.5%) while 13 cases (15.7%) were diagnosed during ambulatory chemotherapy treatment. None of the patients with CAT received prophylaxis anticoagulant during cancer treatment or follow up period. Characteristics of patients with CAT are summarized in Table 1.
Of 83 patients with CAT, 66 patients were treated with anticoagulants, while inferior vena cava filter was used in 8 patients (9.6%). The cumulative incidence of total bleeding events at 1 year was 21.1% whereas cumulative incidence of major bleeding was 6.8%. The cumulative incidence of recurrent thrombosis at 1 year was 8.3%.
Cancer patients who developed CAT had both a significantly higher NRM (26.2% vs. 13% at 1 year, p=0.004) (Figure 1A) and relapse rate (63.3% vs. 43.5% at 5 years, p=0.002) (Figure 1B) when compared with control group, which resulted in a significantly lower 5-year OS (24.9% vs. 62.7%; p<0.0001) (Figure 1C) and PFS (16.9% vs. 46%; p<0.0001) (Figure 1D).
Advanced stage cancer and development of CAT were associated with poor OS in a multivariable analysis with HR of 6.9 (95%CI 2.7-17.7) and 3.9 (95%CI 2.2-7.0), respectively. Both factors also independently predicted risk of relapse with HR of 4.6 (95%CI 1.8-11.6, p=0.001) and 3.4 (95%CI 1.7-6.8, p<0.0001), respectively.
Conclusions
Development of CAT is associated with an increased NRM, relapse rate and poor survival in patients with cancer. Effective strategies to prevent CAT especially in high-risk cancer patients are needed to help improve outcomes.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal